Access to Health Care: Free, but for all? Nearly nine million Canadians report chronic difficulty getting help
by David Korzinski | September 6, 2022 10:00 pm
Canadians say they have less confidence and more difficulty accessing health care than Americans
September 7, 2022 – A summer of health care related horror stories – from emergency room closures to doctor shortages to surgery delays – is shaking public faith in what has traditionally been a source of national pride[1].
A comprehensive new cross-border study of Canadians and Americans from the non-profit Angus Reid Institute finds those north of the border dealing with considerably more difficulty in accessing care. This is the first in a three-part series canvassing opinion on access to, quality of, and policy towards health care in Canada.
It finds that over the last six months, two-in-five Canadians (41%) – approximately 12.8 million adults – say they either had a difficult time accessing or were totally unable to access one of five key health services: non-emergency care, emergency care, surgery, diagnostic testing, and specialist appointments.
Americans are much less likely to say they encountered barriers to accessing those services, despite near-identical levels of the population seeking this type of care – 70 per cent in the United States and 74 per cent in Canada.
Asked how confident they feel that they could access urgent care in a timely fashion if a household emergency arises, 37 per cent of Canadians are confident while 61 per cent are not. In the United States, 70 per cent are confident, while one-quarter (25%) are not.
To better synthesize a significant amount of response data, Angus Reid Institute researchers created a Health Care Access Index, which finds the smallest group – 15 per cent of the population – enjoying Comfortable Access (approximately 4.7 million Canadian adults). The rest of the country is divided into three groups – those facing Some Challenges (31% – 9.7 million), Chronic Difficulty (29% – 9 million), and those not requiring access during this period (26% – 8.1 million).

More Key Findings:
- Americans are twice as likely as Canadians to report Comfortable Access to health care – 30 per cent compared to 15 per cent respectively.
- In Canada, young women and young men are most likely to be found in the Chronic Difficulty group, compared to their older peers. British Columbians and Atlantic Canadians are also overrepresented in this most challenged category of health care seekers.
- Among those who had easy or very easy access to surgery, 55 per cent say their health has improved over the past six months. Three-in-ten (28%) say their health has stayed the same, while 17 per cent report it as having worsened. Those who had a difficult or impossible experience accessing this type of care are twice as likely (34%) to say their health has worsened since.
About ARI
The Angus Reid Institute (ARI) was founded in October 2014 by pollster and sociologist, Dr. Angus Reid. ARI is a national, not-for-profit, non-partisan public opinion research foundation established to advance education by commissioning, conducting and disseminating to the public accessible and impartial statistical data, research and policy analysis on economics, political science, philanthropy, public administration, domestic and international affairs and other socio-economic issues of importance to Canada and its world.
Part One: Canadian Health Care Access: Personal experiences over the past six months
-
Equal access in concept, not in practice
-
Challenges impact outcomes
-
Seven-in-ten say friends, family face challenges to access
-
What if you had an emergency?
Part Two: The Health Care Access Index
-
Comfortable Access
-
Some Challenges
-
Chronic Difficulty
-
Didn’t Require Access
-
Access by region
-
Access by age and gender
Part Three: American, Canadian experiences with access
-
Significant differences in experience
-
Confidence in Canadian system comparatively low
Part One: Canadian Health Care Access: Personal experiences over the past six months
Canada’s health-care system has been under intense scrutiny in recent months, as the country looks past COVID-19 to find long[2] waits[3] – or complete closures[4] – at emergency rooms[5], shortages of health-care workers[6], a lack of family doctors[7], and backlogs[8] for surgeries[9]. The health-care system has been described as “collapsing”[10], or “collapsed”[11]. The president of the Canadian Medical Association calls the current pressure on the system “unsustainable”[12], as multiple headlines[13] characterize the situation as a “crisis”[14].
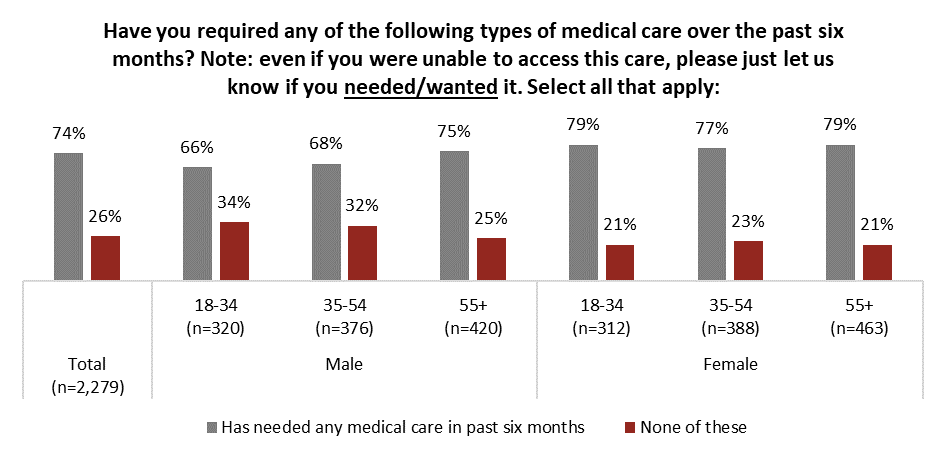
In this current environment, three-quarters (74%) of Canadians say they have required some sort of medical care over the past six months. For most of this group, their care needs were something a family doctor could handle. Other significant segments required a diagnostic test, an appointment with a specialist or something more urgent, as seen in the graph below:

Overall, men are far less likely to report requiring medical care recently, topping out at three-quarters (75%) of men over the age of 54. This confirms previous research[15] which suggests that some men simply do not like going to the doctor, and do so at rates lower than women of the same age. For women, nearly four-in-five in all age groups report needing medical treatment:
Equal access in concept, not in practice
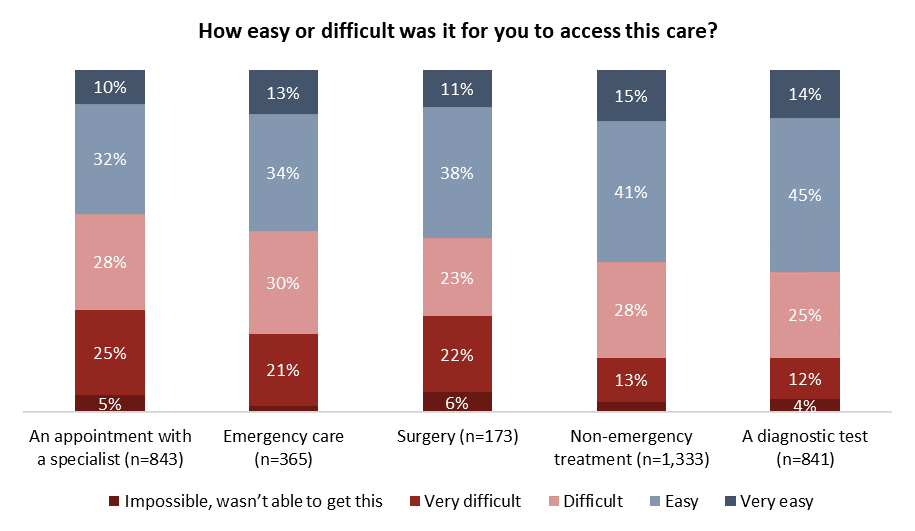
Those who required health care in recent months were then asked how easy or difficult it was to access care. Health care seekers report specialist appointments and surgical procedures caused the most stress, with more than half reporting a difficult time or an impossibility accessing this type of care.
Those who needed non-emergency treatment and diagnostic tests were less likely to encounter barriers. Still, at least two-in-five who needed tests (41%) or non-emergency treatment (44%) say it was difficult or impossible to get them:
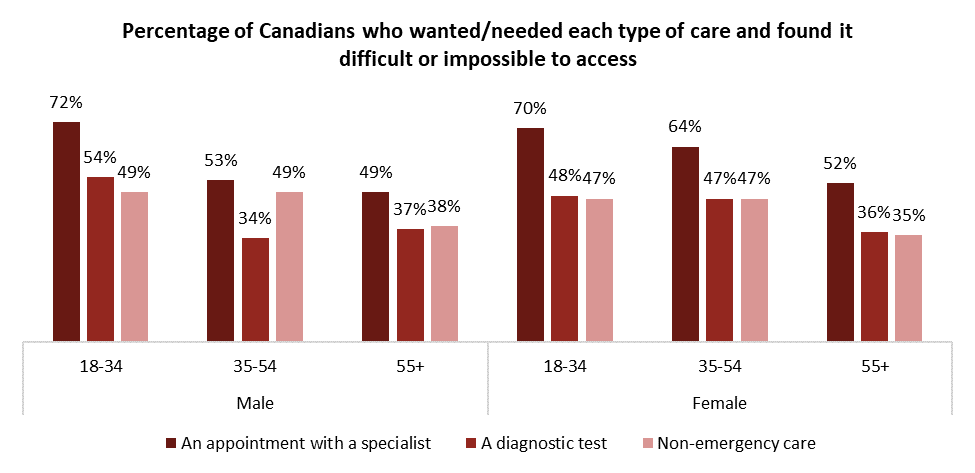
While difficulty accessing non-emergency care from a doctor or walk-in clinic is relatively consistent, younger people report having a much harder time getting in to see a specialist or receive a diagnostic test. As we will see in the forthcoming second release in this ARI health series, the lack of primary care is a key driver of this.
Challenges impact outcomes
While the Angus Reid Institute cannot say problems accessing health services cause poor health outcomes, there is a notable correlation. Those who report challenges getting care are more likely to report that their health has deteriorated in recent months than those who had an easier time getting the health care they needed. In the case of those who needed surgery, a visit to the emergency room, or a diagnostic test, at least twice as many people who had difficulty with access also say their health worsened in the last six months:
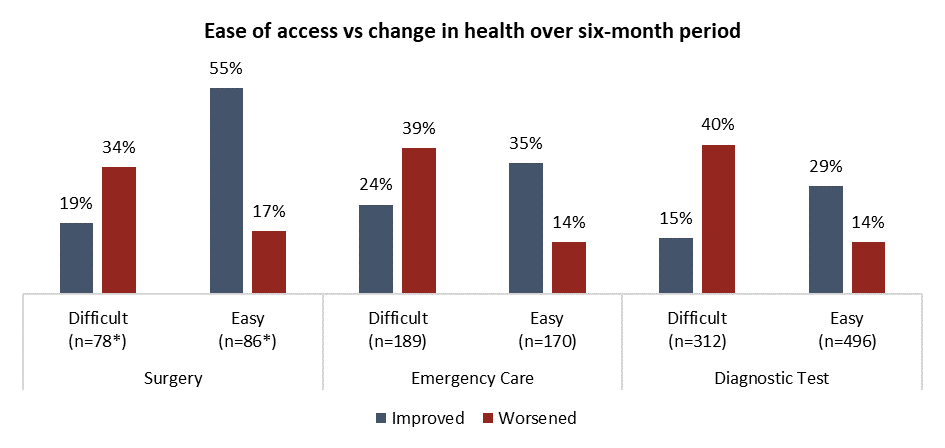
*Smaller sample size, interpret with caution
A similar correlation between ease of access and self-assessment of their own health is seen among those who say they needed specialist appointments or non-emergency care. Three-times as many people who report accessing a specialist was difficult say their health worsened (35%) in recent months when compared to those who instead say seeing a specialist was easy (11%), as seen in the graph below:

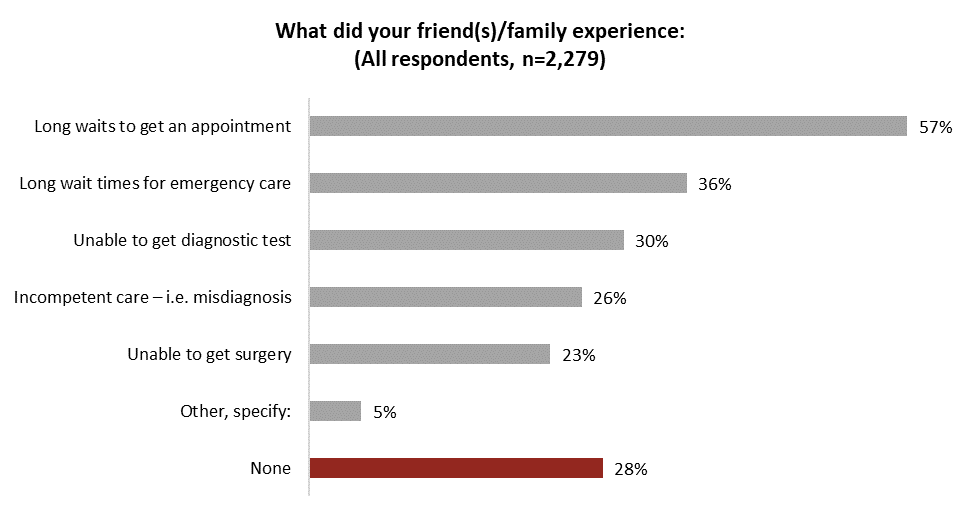
Seven-in-ten say friends, family face challenges to access
The vast majority of Canadians also report having friends or family who were left wanting by their experiences with the health-care system. Nearly three-quarters (72%) say they know at least one person – a close friend or family member – who received inadequate medical care in the last six months (see detailed tables[16]).
Long wait times are the most common health-care concern Canadians report friends and family have experienced. Three-in-five (57%) say loved ones faced lengthy delays to get appointments. One-third (36%) know someone in their circle who faced a long wait-time for urgent care while others were challenged by an inability be scheduled for a diagnostic test or surgery:
Half (51%) of Canadians say someone close to them suffered consequences because of inadequate health care, while one-in-five (18%) say a friend or family member suffered serious consequences because of poor access to health care:

What if you had an emergency?
As stories of poor health care access proliferate, confidence in the system appears to be low among Canadians. Three-in-five (61%) are not confident they, or their family, will be able to get timely access to health care in an emergency, including one-quarter (24%) who have no confidence at all. Two-in-five (37%) are more optimistic they will receive emergency care without delays.
Confidence is lower in Atlantic Canada than elsewhere in the country. Notably, three of that region’s premiers recently met with Ontario Premier Doug Ford[17] to call for health-care changes – including potential private solutions[18] – as the Maritimes’ health system struggles:

Across age and gender demographics, men older than 54 are evenly split on confidence in being able to secure timely care if they were in an emergency. This represents the most optimistic and confident demographic cohort. Men and women across all other age groups are significantly more pessimistic, especially younger women:

Part Two: The Health Care Access Index
To better understand the varied experiences of Canadians over the past six months, Angus Reid Institute researchers created the Health Care Access Index, which used a scoring mechanism to categorize respondents into one of four groups. One of these groups – 26 per cent of Canadians overall – is simply made up of those who have not needed to access care over the past six months. The other three groups are scored based on their interactions with various levels of care. Broadly, positive interactions with health care – accessing health care services or a doctor’s appointment easily – are scored positively and negative interactions – having a difficult time getting care – are scored negatively. For full details on how the Index was scored, please click here[19].
Using this Index, Canadians who needed health care recently fall into one of three groups: those with Comfortable Access, Some Challenges, or Chronic Difficulty in securing adequate care.

Below are some of the demographic and experiential details that help to define each group. Canadians from all walks of life are represented in each, but some have higher concentrations of demographic factors than others. Note that data referenced below involving family doctors or general practitioners, as well as views of the quality of health care within communities, will be released in subsequent waves of this comprehensive three-part series. For now, they are referenced in these group summaries.
Comfortable Access: 15%, equivalent adult population = 4.7 million adults
- None have had a “very difficult” time accessing any of the five health-care services listed
- A handful have had a “difficult” time accessing some services, no more than 9%
- Older (28% over 65, 21% aged 55-64)
- Little to no gender or income difference compared to general population sample
- Slightly overrepresented in Ontario – 43 per cent, highest in any group
- 99% have a family doctor
- Most can see their doctor whenever they like (62%), one-in-three say it takes a couple days
- 61% say health care where they live is “good” or “very good” – only group to say this at a majority level
- 28% believe private care could improve Canada’s system
- 61% confident they could get emergency care if it was needed
Some Challenges: 31%, equivalent adult population = 9.7 million adults
- Two-in-five had a difficult time getting either emergency care or a specialist appointment in past six months
- 98% have a family doctor, but it is difficult to get an appointment: For more than half (53%), it takes a few days; for 43 per cent, it takes more than a week
- Only 37% are confident they could get timely emergency care if needed
- 41% say health care is “good” or “very good” where they live
- Those in Saskatchewan and Ontario more likely to fall into this category than residents in other provinces
Chronic Difficulty: 29%, equivalent adult population = 9 million adults
- At least three-quarters say it’s difficult or impossible to access each of the five types of care listed
- 58% say it was very difficult or impossible to see specialist, 48% say very difficult or impossible to get surgery
- 35% say their health has worsened over the past six months
- 80% say health care is “poor” or “very poor” where they live
- Just 20% confident they could get timely emergency care if needed
- 37% are supportive of more investment in private care
- Youngest group – 35% under 35
- Lowest income levels compared to other groups
- Overrepresented in B.C. and Atlantic Canada
Didn’t Require Access: 26%, equivalent adult population = 8.1 million adults
- Quebecers are overrepresented in this group, one-third in that province say they didn’t require access to health-care system in last six months
- Three-in-five (57%) in this group are men
- Evenly distributed by age: 30% are aged 18-34, 36% aged 35-54, 34% aged 55+
- More than half (55%) say they aren’t confident they would receive timely care in an emergency
- Seven-in-ten (72%) have a family doctor, a higher proportion than those in the Chronic Difficulty group
To truly perceive the scale of the challenges facing those with Chronic Difficulty, consider the proportion of those within the group who have had a difficult time accessing each of the items presented. For those with Chronic challenges, most attempts at accessing care have been difficult or impossible. Among the Comfortable, few faced challenges in finding adequate care:

Among those experiencing Chronic Difficulty with access, the problems compound: three-in-five (60%) have had a tough time accessing two or more types of care in this six-month window. So not only does this group struggle with access to one type of health care, but several, making this group an outlier compared to those in the Comfortable or Some Challenges segments, as seen in the graph below:

Access by region
As mentioned earlier, access issues appear worse in British Columbia and Atlantic Canada, where those with Chronic Difficulty exceed one-third within their respective regional populations:

Access by age and gender
Age and gender combinations generate a starker divide. While all groups experience challenges, those older than 54 years of age are most likely among both genders to have Comfortable Access. Young women are most likely to have Chronic Difficulty in access, followed by young men, who notably, are also least likely to try to access care.

Part Three: American, Canadian experiences with access
The earliest beginnings of universal health care in Canada trace back to the post-war period in Saskatchewan[20], evolving over time through a series of legislation at both the provincial and federal levels into the system we have today. Over the last seven decades, the Canadian health-care system has held up as a point of pride for this nation[21], and a point of envy for Americans who admire[22] it.
In this study, Americans were asked identical questions about their own need of and access to health services in their community. There was no significant difference in the number of Americans seeking care (70% did) relative to the number who needed health care in Canada (74%).

Significant differences in experience
This is largely where that consistency of experience ends. Across every item on the list of services canvassed – non-emergency and emergency care, surgery, appointments with a specialist, and diagnostic tests – Americans are far more likely to say that this service was either easy or very easy to access. Meanwhile, at least two-in-five Canadians had difficulty accessing each.
Prior to the pandemic, Canadians were already much more likely[23] to wait for more than a month for a specialist appointment than Americans. The problem appears to only have grown[24] since the onset of COVID-19:

Applying the same scoring criteria for the Health Care Access Index to Americans, it becomes clear that Canadians are more concentrated on the negative end of the experience spectrum than their southern neighbours. Americans are twice as likely to be Comfortable and half as likely to face Chronic Difficulty. In both countries, the number of those who have Some Challenges or did not require care in the six months prior to this survey, are very similar:

On the question of access however, it is important to address a significant point of methodology: one may question, given the system of private, user-pay health care in the United States, the extent to which access depends significantly on income. While lower income respondents in the United States are more likely than those in higher income brackets to report facing barriers to health care access, the same is true in Canada. It is further worth noting that the national uninsured rate in the United States is at an all-time low as President Joe Biden’s administration made efforts to increase health care access in that country[25].

When it comes to the experiences of their loved ones, Americans are much less likely to say they know someone who faced obstructed, or poor, health care. Canadians are nearly three times as likely as Americans to report a loved one was unable to get a diagnostic test (30% Canadian; 12% American). As well, Canadians are four times as likely (23% vs. 6%) to say they know someone who could not get surgery. Overall, two-in-five (43%) Americans say they know no one in their life who received inadequate health care, more than the three-in-ten (28%) Canadians who say the same:

Confidence in Canadian system comparatively low
Americans are much more confident in their health system than Canadians. A majority (70%) in the United States say they are assured they would get care in a timely fashion in an emergency. Two-in-five (37%) in Canada hold the same belief in their own country’s health-care system:

What’s Next:
The second part of this three-part series will be released in the coming days, and will focus on access to family doctors, and the recent phenomenon of virtual care that many Canadians have experienced during the COVID-19 pandemic.
Survey Methodology:
The Angus Reid Institute conducted two online surveys in August 2022. Sample in Canada was drawn from Angus Reid Forum, while sample in the United States was drawn from Angus Reid Forum USA. The survey was self-commissioned and paid for by ARI.
In Canada: The Angus Reid Institute conducted an online survey from Aug. 8-10, 2022, among a representative randomized sample of 2,279 Canadian adults who are members of Angus Reid Forum. For comparison purposes only, a probability sample of this size would carry a margin of error of +/- 2.0 percentage points, 19 times out of 20.
In United States: The Angus Reid Institute conducted an online survey from Aug. 16-17, 2022, among a representative randomized sample of 1,209 American adults who are members of Angus Reid Forum USA. For comparison purposes only, a probability sample of this size would carry a margin of error of +/- 3.0 percentage points, 19 times out of 20.
For detailed Canadian results by age, gender, region, education, and other demographics, click here[26].
For Canadian results by ease of access to health care services, click here[27].
For detailed American results by age, gender, region, education, and other demographics, click here[28].
For detailed results across the Health Care Access Index, click here for Canada[29] and here for the United States[30].
To read the full report, including detailed tables and methodology, click here[31].
To read the questionnaire in English and French, click here[32].
Image – Marcel Scholte/Unsplash
MEDIA CONTACT:
Angus Reid, Chairman: angus@angusreid.com[33]
Shachi Kurl, President: 604.908.1693 shachi.kurl@angusreid.org[34] @shachikurl
Dave Korzinski, Research Director: 250.899.0821 dave.korzinski@angusreid.org[35]
- source of national pride: https://www.washingtonpost.com/news/worldviews/wp/2018/02/23/canadas-health-care-system-is-a-point-of-national-pride-but-a-study-shows-it-might-be-stalled/
- long: https://www.cbc.ca/news/canada/new-brunswick/new-brunswick-health-care-wait-times-1.6556275
- waits: https://toronto.citynews.ca/2022/08/01/ontario-hospitals-emergency-room-wait-times/
- complete closures: https://ottawa.ctvnews.ca/perth-ont-hospital-er-reopens-after-three-week-closure-1.6000002
- emergency rooms: https://globalnews.ca/news/9066662/emergency-rooms-canada-big-small/
- shortages of health-care workers: https://www.cbc.ca/news/politics/healthcare-workers-burnout-1.6492889
- a lack of family doctors: https://www.cbc.ca/player/play/2052889667732
- backlogs: https://www.cbc.ca/news/canada/prince-edward-island/pei-surgery-wait-times-2022-1.6538585
- surgeries: https://www.cbc.ca/news/canada/calgary/surgeries-backlog-saskatchewan-alberta-von-scheel-1.6556962
- collapsing”: https://www.ctvnews.ca/health/canada-s-health-care-system-is-collapsing-around-us-warns-cma-president-1.5948416
- “collapsed”: https://globalnews.ca/news/8998826/er-doctors-health-system-collapsed-patient-surges-emergency-room-closures/
- “unsustainable”: https://globalnews.ca/news/9071575/code-blue-canada-health-care-crisis-series/
- headlines: https://nationalpost.com/opinion/kelly-mcparland-health-care-is-canadas-most-pressing-crisis-yet-our-politicians-are-largely
- “crisis”: https://globalnews.ca/news/9071575/code-blue-canada-health-care-crisis-series/
- previous research: https://www.huffpost.com/entry/why-men-dont-go-to-the-doctor_n_5759c267e4b00f97fba7aa3e
- see detailed tables: https://angusreid.org/wp-content/uploads/2022/09/2022.09.01_Health_Part_1_tables.pdf
- met with Ontario Premier Doug Ford: https://www.cbc.ca/player/play/2064520259924
- potential private solutions: https://atlantic.ctvnews.ca/premiers-hint-at-health-care-changes-but-workers-say-public-system-should-be-fixed-first-1.6039605
- please click here: https://angusreid.org/wp-content/uploads/2022/09/Health-care-access-index.pdf
- the post-war period in Saskatchewan: https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/health-care-system/canada.html
- a point of pride for this nation: https://edmontonjournal.com/opinion/columnists/paula-simons-american-tweet-prompts-canadian-love-in-for-public-health-care
- admire: https://www.gao.gov/assets/hrd-91-90.pdf
- already much more likely: https://www.oecd-ilibrary.org/sites/242e3c8c-en/1/3/2/index.html?itemId=/content/publication/242e3c8c-en&_csp_=e90031be7ce6b03025f09a0c506286b0&itemIGO=oecd&itemContentType=book
- have grown: https://globalnews.ca/news/9086399/canada-orthopaedic-surgery-backlog/
- in that country: https://www.hhs.gov/about/news/2022/08/02/new-hhs-report-shows-national-uninsured-rate-reached-all-time-low-in-2022.html
- click here: https://angusreid.org/wp-content/uploads/2022/09/2022.09.01_Health_Part_1_tables.pdf
- click here: https://angusreid.org/wp-content/uploads/2022/08/2022.08.31_Health_Part_1_access_tables.pdf
- click here: https://angusreid.org/wp-content/uploads/2022/08/2022.08.31_Health_Part_1_US_tables.pdf
- click here for Canada: https://angusreid.org/wp-content/uploads/2022/08/2022.08.31_Health_Part_1_index_tables.pdf
- here for the United States: https://angusreid.org/wp-content/uploads/2022/08/2022.08.31_Health_Part_1_US_index_tables.pdf
- click here: https://angusreid.org/wp-content/uploads/2022/09/2022.09.07_HC_Part_1.pdf
- click here: https://angusreid.org/wp-content/uploads/2022/09/2022.09.07_Health_1_qnnaire.pdf
- angus@angusreid.com: mailto:angus@angusreid.com
- shachi.kurl@angusreid.org: mailto:shachi.kurl@angusreid.org
- dave.korzinski@angusreid.org: mailto:dave.korzinski@angusreid.org
Source URL: https://angusreid.org/canada-health-care-issues/